The first full description of Progressive supranuclear palsy (PSP) occurred in 1964. PSP begins during the late 50s to mid 60s (earliest reported age 43). Men are slightly more frequently affected than women. Median survival is under 10 years. PSP accounts for about 5% of patients in a typical movement disorders centre. PSP is not a synucleinopathy like Parkinson’s disease, Dementia with Lewy bodies (DLB) or Multiple system atrophy (MSA), but a rather a tauopathy, relating it more with Cortical basal degeneration (CBD).
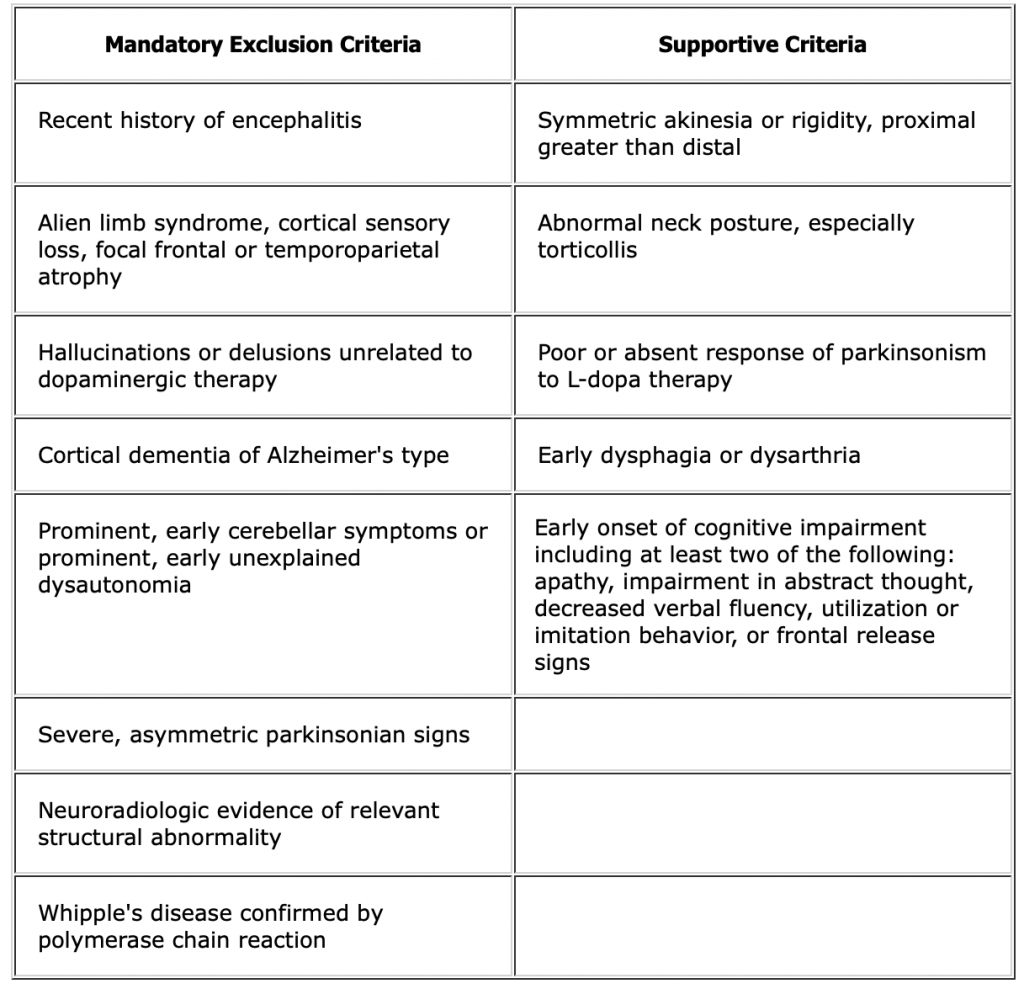
40% to 50% of patients will have an initial mild, transient response to levodopa … but the response to levodopa is not as robust in these patients as it is in patients with Parkinson’s disease.
The typical supranuclear eye movement abnormalities are often not seen until four years after the onset of the other symptoms. These begin as an impairment of down or upgaze. This can be picked up early by checking vertical optico-kinetic nystagmus. Associated ocular findings are horizontal square-wave jerks, slow and hypometric saccades, apraxia of eyelid opening, blepharospasm, or a severely reduced blink rate and a progressive paresis of gaze in all directions.
Expect an early disorder of gait with falls in over 60% to 90%. This is due to early loss of postural reflexes.
Axial rigidity particularly in the neck may be associated with hyperextension, causing a retrocollis. Limb tone may be only mildly increased, increasing from proximal to distal, and is typically more symmetric by comparison to Parkinson’s disease. Dystonia of facial muscles create a recognizable pattern of a surprised, wide open eyes look. Tremor is uncommon (5 – 10%) and is evident more often with posturing and action. Personality and cognitive changes occur frequently and early. These changes include emotional incontinence, irritability, and social withdrawal. Moderately severe dementia is common.
By 5 years, 68% of patients have significant speech dysfunction … some may progress to anarthria. 46% are affected by dysphagia within 5 years. Sleep disturbance is common. Autonomic failure is less common than in Parkinson’s disease with the exception of incontinence.
For more information and support/resources:
- Cure PSP: http://www.psp.org
- NIH PSP Information page: http://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Progressive-Supranuclear-Palsy-Fact-Sheet