Parkinson’s Disease is a sporadic disorder, with a probable genetic predisposition in ~16% of families. Conservative estimates indicate that 2% of the general population will develop Parkinson’s by age 80. The average age of onset of symptoms is 63. The range of age of onset is quite wide, with “young onset” Parkinsons occurring not infrequently. 8% of patients have the onset of their symptoms before age 40.
There are no blood tests or X-rays that will confirm the diagnosis. although PET scans are capable of detecting a deficiency in some forms of Parkinsonism. The diagnosis is based on meeting specific motor criteria (established by the United Kingdom Brain Bank Criteria) and ruling out other possible causes including several conditions that can mimic Parkinson’s Disease but often have additional features (Atypical Parkinsonisms or Parkinson’s “Plus” syndromes).
Motor symptoms
1 – Tremor
This is present in 80% of cases. It is usually manifest by a tremor at rest (at a time when the body part is relaxed). It may affect the hands, feet, chin, and tongue. It can be brought out by distraction such as mental arithmetic. It doesn’t affect the head.
Classically when it affects the hand it creates a “pill rolling” tremor. The thumb slides back and forth on the index finger. The tremor will in time progress to involve muscles at the wrist, then the forearm and then the arm. 30% of patients will also have a component of this tremor with action (movement induced tremor). This tremor, like all tremors, will be worse after physical exertion, with fatigue or with good and bad emotional excitement.
2 – Rigidity (stiffness)
Rigidity or stiffness in muscles leads to a characteristic loss of arm swing with walking, loss of facial expression, fatigue, and a variety of muscle pain syndromes (e.g. frozen shoulder). This is identified on examination by the examiner passively manipulating the limb while the patient is relaxed. Getting the patient to perform movements with the opposite side of the body will accentuate the abnormality in the tone of the limb. There is a classically described “cog-wheel” type of rigidity in Parkinson’s Disease.
Without regular exercise, physiotherapy, and/or medication this rigidity can lead to progressive problems with immobility and muscular pain.
3 – Bradykinesia (slow movement)
A general slowing down of movement will occur. The features that should be looked for include slowness of speed, loss of amplitude over time and a disruption in a smooth rhythm. Eventually there may be hesitations and “freezing” of movement. This together with the rigidity is responsible for much of the disability that occurs as a result of Parkinson’s disease. The walking slows, the feet start to shuffle, the voice softens, and the face losses its expression. Fine coordinated tasks like buttoning and cutting food become difficult. Writing becomes messy, and gets smaller, and increasingly illegible.
4 – Other motor symptoms
There is a typical gait disorder (click on the hyperlink for an excellent YouTube video example) that starts with loss of arm swing on one side then the step length shortens and walking speed slows down. The body becomes more stooped or flexed and the arms bend more at the elbows – gradually this worsens with increasing difficulty getting started (gait initiation hesitation) and turning (en bloc turning).
- A stooped posture and a blank facial expression occurs as the result of immobility and rigidity.
- Postural instability (loss of balance) occurs later in this condition.
- Freezing (sudden loss of movement) often occurring in narrow passages such as doorways; attempting a movement that requires more than one action (such as walking to a door and opening it) may also trigger this. Cues such as seeing something to step over, hearing a beat to move with, or having someone touch the individual may help the person to start moving.
- Speech problems result from incoordination or reduced movements of the muscles involved in breathing, voice, pronunciation and prosody (rhythm, intonation and speaking rate). The first change is usually a soft or fading voice. Words may become slurred or unclear with the final sounds in words being omitted. Speech may become faster. There may be difficulty beginning conversations or sentences causing hesitations or uncontrolled repetitions of words or phrases. Drooling may cause muffled speech.
- Difficulty swallowing affects approximately 50% of advanced Parkinsonians. It is caused by slow moving, poorly coordinated throat muscles
Non-motor symptoms
We now know in addition to the more often recognized motor symptoms, that a host of additional “non-motor” problems arise in this condition …. many of these are symptoms are evident years before the motor symptoms develop. It is common for constipation, loss of sense of smell, sleep disorders and anxiety to precede the motor symptoms and have been reported to do so up to 20 years prior to the motor diagnosis.
- Loss of smell – one of the earliest symptoms
- Sleep disorders include:
- REM (rapid eye movement) sleep behaviour disorder – a condition during which patients while dreaming abnormally retain the ability to move and can be seen “acting out their dreams”. This can be dangerous as it can lead to sleep related falling out of bed or unintentionally striking one’s bed partner while dreaming.
- Restless Leg syndrome (RLS) – a condition where when the patient relaxes, typically while lying down at night to fall asleep they get an uncomfortable sensation in their legs associated with an urge to move the legs to obtain relief.
- Sleep fragmentation – a result of frequent nocturnal wakening secondary to a variety of causes including; urge to go to the bathroom to urinate, muscular cramping, difficulty rolling over in bed, nightmares, REM sleep problems, nocturnal wearing off related to Parkinson medications not lasting through the night, early morning wakening (sometimes a sign of depression). This leads to or contributes to daytime sleepiness.
- Sleep Apnea – is reported in up to 30% of patients with Parkinson’s disease. It results from a combination of either an obstructive component which occurs as a result of a relaxation of the jaw and throat muscles allowing the patient’s airway to be obstructed, or a loss of the central drive to breath at certain stages of sleep. This causes frequent nocturnal sleep stage disruption and results in a failure of a normal amount of the deep restorative sleep that is required to feel awake during the day.
- Easy fatigability is often the result of the effort and constant attention required to move. This is complicated by sleep disturbances including sleep initiation problems and early morning wakening that may result from depression. Insomnia may occur as a side effect of anti-Parkinson’s medication, as can vivid dreams or nightmares.
- Constipation is often a major problem. It results from a combination of immobility, dehydration, and slowing of motility. This can lead to early satiety, loss of appetite and eventually weight loss.
- Loss of the sense of thirst is common in Parkinson’s disease and contributes to low blood pressure symptoms and constipation.
- Drooling is often an early symptom with the pillows being wet at night. This isn’t due to increased salivation, but relates to decreased frequency of swallowing.
- Autonomic Dysfunction
- Sexual dysfunction is common
- Sweating, or an impaired sweating response may occur. Anti-Parkinson’s medications may aggravate this. It most commonly happens when the benefit of Parkinson’s medications wears off (e.g. the middle of the night)
- Abnormal thermal regulation (e.g. feeling cold when in fact the environment is warm or vice versa)
- Orthostatic hypotension – a sensation of light-headedness which occurs either immediately or after 1-2 minutes upon rising to a standing position from a sitting/lying down position. If severe enough, the accompanying loss of blood flow to the brain can result in passing out (e.g. fainting) and falling, potentially resulting in injury. Problems with low blood pressure may also cause neck pain, blurred vision and confusion.
- Bladder problems – results from varying effects of the illness on sphincter muscle control – typically, this results in increased urgency and frequency of urination, particularly at night. Anti-Parkinson’s medications may cause retention of urine.
- Seborrhea or excessive scalp, eyebrow or eyelash oiliness, reddness, or scaliness may occur.
- Mental changes including depression which occurs in approximately 30% of Parkinson patients may be aggravated by self-imposed social isolation. Fatigue may contribute to feelings of discouragement, and lead to apathy. Anxiety may also be evident.
- Mental slowing – progressive difficulty with attention and poor working memory, can progress to dementia after several years in 30-40%
- Memory loss will occur in up to 30-50% of patients. Short term memory is usually affected first.
Cause
The cause is unknown but assumed to be the result of a combination of environmental influences (toxins, infections) superimposed on a varying genetic predisposition/ susceptibility. Findings recently suggest the illness has its origins in the gut (enteric nervous system) and then spreads into either the lower brainstem (vagal nerve controlling bowel function) and/or the olfactory nerves (loss of sense of smell) and either spread or gradually develop in adjacent regions (brainstem involvement likely contributes to anxiety and sleep disorders) until the substantia nigra in the midbrain is affected. At this stage the motor symptoms become evident. It is known that all Parkinson patients have a marked reduction in the number of nerve cells in the substantia nigra. Some families are known to be have an inherited defect that is assumed to result in a failure of survival of these nerve cells. These cells are known to die off earlier than expected in Parkinson’s Disease. This results in the chemical that these cells produce, dopamine, becoming deficient. Without dopamine, the part of the brain that normally slows down excess movement becomes over active, resulting in the slowness and stiffness seen in this disorder.
Researchers still don’t know why but there is increasing evidence that the variety of genetic and environmental insults leading to Parkinson’s have in common, a collection of abnormal forms of a normal protein – alpha synuclein – this seems to contribute to death of brain cells. There are some who feel that this protein, when it is in an abnormal state, can spread from cell to cell causing further nerve cell loss. Research is exploring ways of controlling the production or improving the clearance of this protein.
Treatment
There are currently several options to treat Parkinson’s disease.
The first step is to make sure the patient becomes well informed about the disorder and has a doctor with experience in managing this condition. An interdisciplinary team approach (involving occupational therapists, physical therapists, speech/language/swallowing therapists, social worker, and dieticians) can be valuable.
Work toward a healthier lifestyle
A healthy lifestyle with good eating, sleeping, and exercise habits is strongly encouraged. To date there is no medication generally thought proven to be able to slow down the progressive nature of Parkinson’s disease. If there was we would want to start it as soon as we know someone has or is at risk of having Parkinson’s dissease.
Exercise is recommended in hopes this may have that potential. 3 hours of cardiovascular fitness producing exercise per week is often recommended. This needs to be vigorous enough to cause an alteration in breathing enough that is would be difficult to carry on a conversation. Any such exercise program should be introduced slowly and with the advise of a physician or physiotherapist – thus, early assessment by a physiotherapist to initiate an appropriate regular exercise program is reasonable.
Treating symptoms
The 2 main options for treatment include replacing dopamine directly with Levodopa or using a chemical mimic of dopamine (a dopamine “agonist”).
As dopamine given directly is poorly absorbed, the medication Levodopa, a precursor of dopamine, which is well absorbed is used). Levodopa is metabolized quickly in the body preventing much of this medication from getting to the brain where it is needed. As a result it is combined with another medication (carbidopa or benzarazide) to allow an effective amount to get into the brain. These other chemicals also reduce the nausea and low blood pressure that would occur if Levodopa was given alone. These medications come under the trade names of Sinemet, Sinemet CR, and Prolopa. Common side effects include nausea, dizziness, and confusion. hallucinations, and abnormal involuntary movements. Domperidone is a medication available in Canada that is very effective at controlling the nausea or low blood pressure if these are persistent problems preventing a patient from tolerating the levodopa.
There are 3 oral dopamine agonists available in Canada, each varying in cost, duration of action, and side effects … in general the side effects are similar to levodopa but more frequent. The dopamine agonists available include: Bromocriptine, Ropinirole, and Pramipexole. A forth dopamine agonist called rotigotine (Neupro) is available as a transdermal patch – the transdermal route of administration allows for smoother delivery of the medication and potentially fewer side effects than the oral versions. Dopamine agonists have the advantage over levodopa in younger patients of reducing the potential of producing dyskinesias and as a result are often suggested early on in management.
After the release of Ropinirole, and Pramipexole, two newly recognized side effects became evident that are very important to watch for:
- The first was excessive daytime sleepiness. In some cases this was associated with sudden onset of sleep (aka “sleep attacks”) and was associated with motor vehicle accidents due to falling asleep at the wheel. All patients need to be aware that this potential exists with all anti-Parkinson medications … should they be experiencing excessive sleepiness during the day (a score of greater than 7 on an Epworth scale) or have any experience of falling asleep in inappropriate circumstances (driving / while eating, or during a conversation) they should immediately stop driving and consult their doctor.
- The next side effect of these medications to be identified relates to impulse control disorders. These include but are not limited to gambling, shopping addiction, eating binges with weight gain, and hypersexuality. Almost any activity that brings a reward can be accentuated and take over one’s normal activities. Should a personality change occur relating to a patient seemingly driven to one or two activities at the exclusion of more normal life interests, their doctor should be notified. The offending medication often needs to be discontinued to resolve this problem.
Other medication options include some older medications such as Amantadine which, interestingly, is the only comoonly used anti-Parkinson medication that can be used to treat dyskinesia (this medication may also help with freezing of gait). Amantadine will help symptoms 60% of the time. It’s duration of benefit varies.
The anti-cholinergics (e.g. trihexyphenidyl, benztropine, ethoproprazine) can be helpful for refractory tremor, and tend to dry up saliva, so they can also reduce drooling. Overall these medications are less well tolerated particularly in older patients due to their tendency to reduce memory and worsen constipation.
Several medications can be given along with Levodopa to prolong its action in the brain. Selegiline and rasagiline are medications that blocks the breakdown of dopamine by the enzyme monamine oxidase type B. Entacapone is another medication that prolongs the life of dopamine in the brain by inhibiting another enzyme responsible for its breakdown (COMT). It is available as a combination pill with levodopa/carbidopa, called Stalevo.
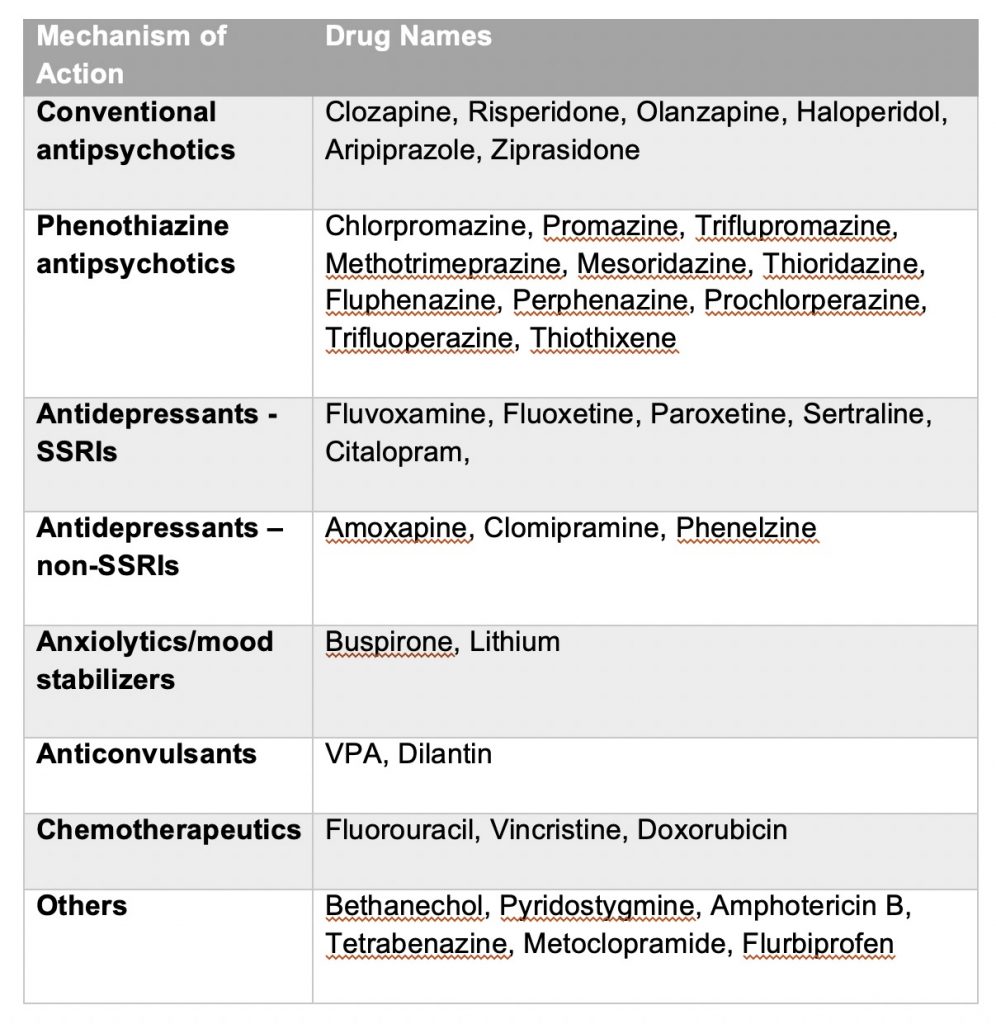
Avoid drugs that are contraindicated in Parkinson’s disease
The term “contraindicated” essentially means that the drug in question should not be given to a patient. Many drugs alter the brain’s dopamine system and may not be recognized as having the potential to markedly alter the symptoms of Parkinson’s simply because the drugs are often used for the treatment of non-neurological conditions. Every patient with Parkinson’s should have a list of these agents available for their physician’s reference:
Surgical options
In addition to pills surgical treatments are now more frequently used to help control symptoms that become refractory to medications:
1 – Stereotactic thalmotomy is a procedure that surgically destroys the very small area deep within the brain that causes the tremor (the thalamus). This, if successful, will stop the tremor on the opposite side of the body. There are, as with any surgery, possible side effects that need to be discussed and considered. Recently non-invasive methods have been developed using ultra-sound based technology.
2 – Deep brain stimulator – is a procedure where a small small electrode is implanted into the globus pallidus or more commonly the subthalamic nucleus. The wire is connected to a programmable transmitter under the chest wall (like a pacemaker). By electrically interfering with the natural firing pattern of the nerve cells in this area, tremor is electrically suppressed. In addition, the rigidity and slowness of movement also improves.
On average with this type of surgery there is an average 50% reduction in the amount of medication a person is taking and a smoothening out of the fluctuations in response to medication. There has now been > 16 years of follow-up and many examples of maintained improvement over the long term. There are, as with any surgery, possible side effects that need to be discussed and considered.